http://www.bjj.boneandjoint.org.uk/content/96-B/2/237.abstract
Arthroscopic debridement in the treatment of patients with osteoarthritis of the elbow, based on computer simulation
- K. Shimada, MD, PhD, Orthopaedic Surgeon, Division Chief2;
- K. Oka, MD, PhD, Orthopaedic Surgeon, Assistant Professor1;
- H. Tanaka, MD, PhD, Orthopaedic Surgeon, Assistant Professor1;
- K. Sugamoto, MD, PhD, Orthopaedic Surgeon, Professor3;
- H. Yoshikawa, MD, PhD, Orthopaedic Surgeon, Professor1; and
- T. Murase, MD, PhD, Orthopaedic Surgeon, Associate Professor1
+ Author Affiliations
- 1Osaka University Graduate School of Medicine, Department of Orthopaedic Surgery, 2-2 Yamadaoka, Suita, Osaka 565-0871, Japan.
- 2Osaka Koseinenkin Hospital, Department of Orthopaedic Surgery, 4-2-78 Fukushima, Osaka 553-0003, Japan.
- 3Osaka University Graduate School of Medicine, Department of Orthopaedic Biomaterial Science, 2-2 Yamadaoka, Suita, Osaka 565-0871, Japan.
- Correspondence should be sent to Dr J. Miyake; e-mail: miyake-osk@umin.ac.jp
Abstract
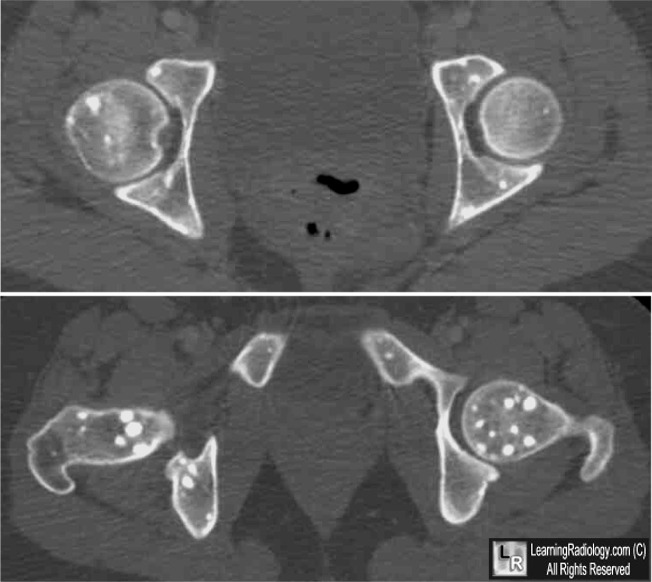
We retrospectively assessed the value of identifying impinging osteophytes using dynamic computer simulation of CT scans of the elbow in assisting their arthroscopic removal in patients with osteoarthritis of the elbow. A total of 20 patients were treated (19 men and one woman, mean age 38 years (19 to 55)) and followed for a mean of 25 months (24 to 29). We located the impinging osteophytes dynamically using computerised three-dimensional models of the elbow based on CT data in three positions of flexion of the elbow. These were then removed arthroscopically and a capsular release was performed.
The mean loss of extension improved from 23° (10° to 45°) pre-operatively to 9° (0° to 25°) post-operatively, and the mean flexion improved from 121° (80° to 140°) pre-operatively to 130° (110° to 145°) post-operatively. The mean Mayo Elbow Performance Score improved from 62 (30 to 85) to 95 (70 to 100) post-operatively. All patients had pain in the elbow pre-operatively which disappeared or decreased post-operatively. According to their Mayo scores, 14 patients had an excellent clinical outcome and six a good outcome; 15 were very satisfied and five were satisfied with their post-operative outcome.
We recommend this technique in the surgical management of patients with osteoarthritis of the elbow.
Cite this article: Bone Joint J 2014;96-B:237–41.
Footnotes
- We thank Ryoji Nakao, computer programmer; Sumika Ikemoto, clinical assistant at the Department of Orthopedic Surgery, Osaka University Graduate School of Medicine; Hisao Moritomo, MD, PhD at the Department of Physical Therapy, Osaka Yukioka College of Health Science; Nobuyuki Kubo, MD at the Department of Orthopedic Surgery, Yukioka Hospital; Eiji Sogo, MD at the Department of Orthopedic Surgery, Kita-Osaka Police Hospital, for their contributions to this study.No benefits in any form have been received or will be received from a commercial party related directly or indirectly to the subject of this article.This article was primary edited by P. Baird and first-proof edited by J. Scott.
- Received August 18, 2012.
- Accepted October 22, 2013.
- ©2014 The British Editorial Society of Bone & Joint Surgery